With the growing demand for healthcare services, the need for skilled physicians, billers, coders, and medical credentialing specialists is on the rise.
Overall employment in the field is projected to grow 13% from the current year to 2031. The expected growth will accommodate 2 million people over the decade.
Let’s look at the statistics of medical credentialing services solely. You will be surprised to learn that this area has witnessed an unexpected growth from USD million to USD multi-million from the year 2017 to 2022.
So if you have an eye for detail, outstanding communication skills, and a keen interest in medical terminologies, you could have a lucrative career as a medical credentialing specialist.
What are medical credentialing services?

Medical credentialing is a two-part process; credentialing and privileging. The first one involves verification of education, competency, licensing, training, and work experience.
The latter is about approving healthcare providers to conduct and perform the procedures they hold expertise.
What is the medical credentialing process?
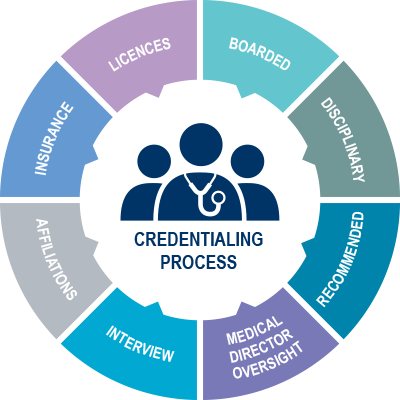
Medical credentialing is a market-driven procedure done to maintain quality standards in the healthcare industry for the patient’s welfare.
The process includes direct communication with the healthcare and insurance providers regarding their qualifications and work.
To verify the educational details, the credentialing authority, also called Credentialing Verification Organization, contacts the university from where the healthcare specialist earns their degree, completes their training, and does their residency to verify their degree.
Moreover, credentialing services also contact certain certification boards as well as licensing agencies to check the legitimacy of specialty certifications and licenses.
Work history is typically obtained from past employers and workplaces. While credentialing is for new hires, the process doesn’t stop even after onboarding to conform to federal and state regulations.
What does a medical credentialing specialist do?
Medical credentialing specialists work in the healthcare industry to ensure that the professional and the organization comply with federal and state regulations.
Medical credentialing specialists possess exceptional communication skills since they must communicate with healthcare professionals and insurance companies regarding amendments in the contract and policies.
Besides that, a medical credentialing specialist must be detail oriented and proficient with relevant computer software.
Also, since this job requires the preparation and maintenance of medical records and activities like accreditation, facility privileges, or memberships, solid written communication is a must.
The medical credentialing specialist has a crucial role as his/her job involves the verification of certifications and ensuring that physicians and facilities are compliant with federal and state guidelines.
Apart from that, they also maintain training and certification proofs for other medical staff. Therefore, a medical credentialing specialist must be efficient with medical terminologies and have exceptional research and organizational skills.
How to become a medical credentialing specialist?
As the Bureau of Labor Statistics (BLS) expects high growth in the medical domain till the year 2030, you can opt for this career path for a secure future.
Surprisingly, you don’t require formal education to become a medical credentialing specialist. It would be enough to gain a bachelor’s degree in health information management, healthcare administration, medical terminology, or other related fields.
Most candidates who want to pursue medical credentialing start their career with a job as a medical administrator.
They need to become proficient in medical terminologies and learn how to research certifications to boost their profile.
As they move forward with their experience and certifications, the next step is to learn federal and state regulations as well as quality assurance standards for certified medical professionals to detect fraud.
Responsibilities of a medical credentialing specialist:
- Streamline the onboarding process for medical staff
- Facilitate the onboarding process by coordinating with Medical Directors, HR/Payroll, Lifespan support staff, and Provider Support Team, including IT, to ensure that all the new joiners have the necessary tools and information needed to function in their respective roles.
- Ensuring the new staff know their orientation schedules and are done with all necessary onboarding tasks, such as paperwork, policy, and health compliance, to meet their effective job date.
- Monitoring, documenting, and reporting each candidate’s status during the hiring process.
- Look into issues to ensure all the deadlines are met
- Prepare and provide any necessary orientation material to HR
- Serve as a focal point for answering queries during the onboarding process.
- Create and maintain NPI forms for all healthcare professionals as well as APPs to add all provider numbers
- Keeping HR, RIH/TMH, MSO, Lifespan Risk Services, Brown EM’s Billing and Coding Departments, and Provider Support Team of credentialing status.
- Track licenses and send monthly reminders to the staff for any expiring licenses.
- Track the certifications of the medical staff and inform them when they require recertifications.
- Track certain vaccinations like influenza shots, to conform to Lifespan’s policies.
- Closely work with the EMUD (Emergency Medicine Ultrasound Director) to ensure all EUS credentialing (initial and reappointment) are met.
These were some of the job responsibilities of a medical credentialing specialist. While there is certainly more to them, we presented you with a summarized list of all the essential ones.
Advantages of Medical Credentialing:

Medical credentialing help the healthcare industry meet its quality standards, benefitting all the partners involved.
For example, facilities can benefit from the patients’ at the cost of their highly skilled and certified staff. In addition, insurance companies benefit from lowering their costs by partnering with facilities that demonstrate quality care for their patients.
Healthcare professionals benefit from it because once insurance companies approve them to accept clients, they can increase their number of patients and generate more revenue.
Finally, care receivers benefit most as they receive the highest quality care.
Conclusion:
Indeed, medical credentialing services are critical jobs in the healthcare industry that only skilled professionals can perform.
To opt for this career path, you must align your educational courses accordingly.
Then, once you have built a solid resume through your education, certifications, and work experience, you can apply for the top healthcare facilities in the United States to get the most out of your education.

Jean Smith is a fitness enthusiast and blogger who focuses on fitness and a healthy lifestyle. She is passionate about assisting people in living healthier lifestyles and is constantly on the lookout for new and creative methods to stay fit and healthy. Her articles are excellent resources for anyone interested in improving their health and fitness.
